Diabetic retinopathy is a serious eye condition that can develop in people with diabetes. It occurs when high blood sugar levels damage the tiny blood vessels in the retina, the light-sensitive tissue at the back of the eye. Over time, this damage can lead to vision loss and even blindness. This is why understanding diabetic retinopathy is crucial for anyone living with diabetes.
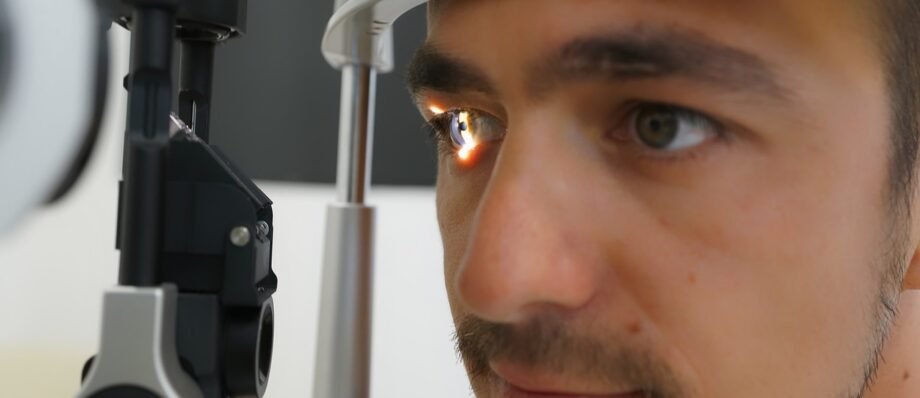
Early detection of diabetic retinopathy is key to preventing vision problems. Regular eye exams are, thus, essential for monitoring eye health and catching any signs of this diabetes eye disease early on.

In this article, we’ll delve into the details of diabetic retinopathy, including its causes, symptoms, risk factors, and treatment options. Let’s work together to protect your vision.
Causes and Risk Factors
How Does Diabetes Lead to Diabetic Retinopathy?
Diabetic retinopathy occurs when high blood sugar levels damage the tiny blood vessels in your retina. These blood vessels can become blocked, leak fluid, or even swell up. Over time, this damage can distort or block your vision. It’s like having tiny pipes in your eye that gradually become clogged or broken.
Risk Factors for Developing Diabetic Retinopathy
Several factors can increase your risk of developing this. Some of these you can control, while others you can’t.
Uncontrollable Risk Factors:
Type of diabetes: People with type 1 diabetes and long-standing type 2 diabetes are at higher risk.
Duration of diabetes: The longer you’ve had diabetes, the greater your risk.
Genetics: A family history can also increase your chances.
Ethnicity: Generally, people of African American, Hispanic, and Native American descent are at higher risk.

Controllable Risk Factors:
High blood sugar levels: Poorly managed blood sugar can accelerate the progression of the condition.
Increased blood pressure: This can worsen damage to blood vessels in the eyes.
High cholesterol: Elevated cholesterol levels can contribute to blood vessel problems.
Pregnancy: Women with gestational diabetes are at increased risk.
Smoking: Smoking damages blood vessels throughout your body. It also includes your eyes.
By understanding these risk factors and taking steps to manage them, you can significantly reduce your chances of developing or worsening condition.
Symptoms of Diabetic Retinopathy
Recognising the Signs of Diabetic Retinopathy
One of the sneakiest things about diabetic retinopathy is that it often doesn’t cause noticeable symptoms in its early stages. This is why regular eye exams are so crucial for people with diabetes. It’s like a silent thief slowly stealing your vision.
However, as it progresses, you may start to experience symptoms. These can include:
Blurred vision: This is a common symptom as the disease advances.
Floaters: These are tiny spots or specks that seem to float in your field of vision.
Dark spots or shadows: These can interfere with your vision.
Vision loss: In severe cases, it can also lead to complete vision loss.

If you notice any of these symptoms, it’s essential to see an eye doctor immediately. And, so, early detection and treatment can help prevent vision loss.
Stages of Diabetic Retinopathy
Progression of Diabetic Retinopathy
Diabetic retinopathy doesn’t just appear overnight. It progresses through several stages. Therefore, understanding these stages can help you appreciate the importance of regular eye exams.
Non-proliferative Diabetic Retinopathy: This is the early stage. Tiny blood vessel damage occurs, causing them to swell or leak fluid. As a result, tiny bulges called microaneurysms may form. While there might be no symptoms at this stage, it’s crucial to catch it early.
Proliferative Diabetic Retinopathy: This is a more severe stage. New blood vessels start growing abnormally in the retina. Furthermore, these new blood vessels are weak and fragile, and they can easily bleed. As a result, this bleeding can lead to vision loss.
Diabetic Macular Edema: This condition occurs when fluid builds up in the macula, the part of the retina responsible for sharp, central vision. It can cause blurred vision and affect daily activities like reading and driving.
It’s important to note that not everyone with diabetes will develop this condition, and the progression of the disease varies from person to person. Regular eye exams are essential for monitoring the condition and catching any changes early on.
Diagnosis and Screening
Detecting Diabetic Retinopathy Through Eye Exams
The only way to detect diabetic retinopathy is through a comprehensive eye exam. This is why regular eye check-ups are so crucial for people with diabetes. It’s like getting a checkup for your eyes.
During a dilated eye exam, your eye doctor will dilate your pupils to get a clear view of the retina. Therefore, they use special equipment to examine the blood vessels and look for signs of damage.
In some cases, your eye doctor may recommend additional tests, such as:
Fluorescein angiography: This involves injecting a dye into your arm and taking pictures of your retina to see how blood flows through the blood vessels.
Optical coherence tomography (OCT): This imaging test provides detailed cross-sectional views of the retina.
Early detection of diabetic retinopathy is key to preventing vision loss. That’s why it’s recommended that people with diabetes have a dilated eye exam at least once a year.
Treatment Options for Diabetic Retinopathy
Managing Diabetic Retinopathy
The cornerstone of managing diabetic retinopathy is controlling your blood sugar levels. Thus, keeping your blood sugar within a healthy range can slow down the progression of the disease. It’s like giving your eyes a break from the harmful effects of high blood sugar.

Additionally, managing other health conditions like high blood pressure and high cholesterol is essential. These conditions can, therefore, worsen damage to the blood vessels in your eyes.
Medical Treatments for Diabetic Retinopathy
Several medical treatments can help manage the condition:
Anti-VEGF injections: These injections target a protein that contributes to blood vessel growth. By blocking this protein, the injections can also help reduce swelling and prevent vision loss.
Steroid injections: These injections can help reduce inflammation in the eye and improve vision.
Laser Surgery for Diabetic Retinopathy
Laser surgery is a common treatment for diabetic retinopathy. It involves using a laser to destroy abnormal blood vessels. There are two main types of laser surgery:
Focal laser treatment: This targets specific areas of the retina where blood vessels are leaking.
Panretinal photocoagulation (PRP): This involves treating a larger area of the retina to prevent new blood vessels from growing.
While laser surgery can help prevent vision loss, it may result in some loss of peripheral vision.
Vitrectomy for Diabetic Retinopathy
In severe cases of diabetic retinopathy, a vitrectomy may be necessary. This surgery involves removing the vitreous gel from the eye and replacing it with a clear fluid. It’s often performed when there’s bleeding in the eye, or if the vitreous gel has become cloudy.
Preventing and Managing Diabetic Retinopathy
Protecting Your Eyes
The best way to protect your eyes from diabetic retinopathy is to manage your diabetes effectively. This involves:
- Maintaining healthy blood sugar levels: Consistent blood sugar control is crucial for slowing down the progression of the condition.
- Managing blood pressure and cholesterol: Keeping these conditions in check helps protect your overall cardiovascular health, including your eyes.
- Regular exercise: Physical activity helps regulate blood sugar levels and improves overall health.
- A healthy diet: Eating a balanced diet rich in fruits, vegetables, and whole grains can support diabetes management.
Coping with Vision Loss from Diabetic Retinopathy
If you experience vision loss due to diabetic retinopathy, know that you’re not alone. Many resources and support systems are available to help you cope.
Low vision aids: These tools can help you with daily tasks.

Support groups: Connecting with others who have similar experiences can provide emotional support and practical advice.
Vision rehabilitation: This therapy can help you learn new skills and strategies for living with vision loss.
Remember, early detection and proper management are key to preventing or slowing down the progression of the condition. By taking care of your overall health and following your healthcare provider’s recommendations, you can significantly reduce your risk of vision loss.
Conclusion
Diabetic retinopathy is a serious eye condition that can significantly impact your quality of life. However, with early detection, proper management, and a proactive approach to your health, you can protect your vision.
Remember, regular eye exams are crucial for people with diabetes. By working closely with your healthcare provider, following an eye care guide, and adopting healthy lifestyle habits, you can take steps to prevent or slow down the progression of the condition.
Your vision is precious – protect it.
FAQ Section
Can diabetic retinopathy be cured?
While there’s no cure for diabetic retinopathy, early detection and treatment can help prevent vision loss and manage the condition effectively.
Is diabetic retinopathy hereditary?
While having a family history of diabetic retinopathy can increase your risk, it’s not directly inherited. Diabetes itself is a primary factor in developing this condition.
What are the early signs of diabetic retinopathy?
In the early stages, diabetic retinopathy often has no symptoms. That’s why regular eye exams are crucial for early detection. However, as the condition progresses, symptoms like blurred vision, floaters, and dark spots may appear.
How often should I get an eye exam if I have diabetes?
The frequency of eye exams depends on the duration and severity of your diabetes. However, it’s generally recommended to have a dilated eye exam at least once a year.
Can diabetic retinopathy cause blindness?
Yes, diabetic retinopathy is a leading cause of blindness among working-age adults. However, early detection and treatment can significantly reduce the risk of vision loss.